Phan Thi Hien, "Esophagus-stomach-duodenum endoscopy in children", Medical Publishing House, Hanoi, Jan 2019 (page 125-137). Extract from specialty book: “NỘI SOI THỰC QUẢN – DẠ DÀY – TÁ TRÀNG TRẺ EM”, Nhà xuất bản y học, Hà Nội, ISBN: 978-604-66-3546-8.
INTRODUCTION
Esophageal stricture can be congenital malformation or secondary to other origins such as postoperative, peptic, caustic, infectieus, postvariceal sclerotherapy and post radiotherapy. In which, postoperative stenosis is a common complication. Achalasia is an esophageal motility disorder that leads to completely or partly losing relaxation of lower esophageal sphincter.In children, these abnormalities can cause complications such as weight loss, malnutrition, food impaction, andinhalation syndrome. Dilatation is a common method to be applied and has a high efficacy in treatment of esophageal stricture and achalasia.
1.ESOPHAGEAL STRICTURE DILATATION
1.1. Indications
Esophageal stricture dilatationis only performed when patients have clinical symptoms of esophageal stricture [1].
Esophageal stricture may appear due to severe reflux esophagitis, especially in children with cerebral palsy [2]. The length of esophageal stricture caused by gastroesophageal reflux is around 1-3cm. The main method is mechanical dilatation before the surgery antireflux [3].
Dilatation method to treat cases with caustic stricture is difficult due to long stricture and many positions. Pneumatic dilation is common application. The indication for caustic stricture causes and its complications has been increased in recent years [4]. If dilatationfailed or esophageal stricture is long with ulcer, an indication for surgery is needed. Common indication of esophageal dilation is due to esophageal stricture after the operation of esophageal atresia.
Congenital esophageal stricture is rare, including 3 groups:membranous webbing, fibromuscular thickening and tracheobronchial remnant. The two first groups can be applied mechanical dilatation, however, it has a high risk of long tear atlocatedstricture [3]. The third group is treated by surgery.
Esophageal dilation requires careful performance in patients with history of perforation or cases who have just done a surgery of upper gastrointestinal tract. Absolutely constraindication of esophageal dilatation is for patients with repeat esophageal perforation [1].
1.2. Technique
Patients need to get esophageal X-ray (to evaluate position, level of esophageal stricture, zenker diverticulum, tracheoesophageal fistula), fasting and antibiotic prophylaxis injection.
1.2.1. Esophageal dilatation by bougie
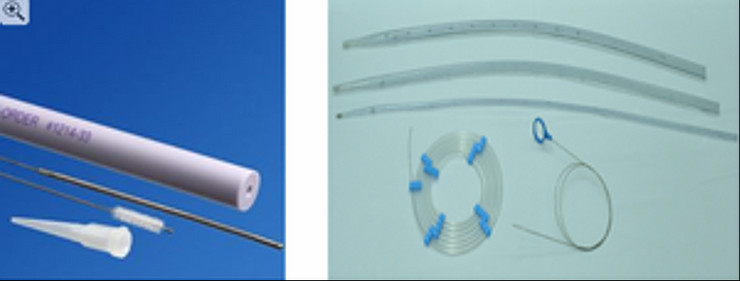
Devices: Savary Dilator with 10 bougies and one metal guide wire with 182cm of length and 0.8mm of diameter. The bougie has 1 cm length is marked by radiologic control [3].
Steps:
- Endoscopy isperform to evaluate stricture position, level and related lesions.
- Insert the soft head of guide wire through the working channel into the stomach and pass structure under observation on endoscopyto avoid perforation or lesion of gastrointestinal tract, then check byC-am to know if it comes into the stomach or not.
- Withdraw the endoscope and remain the guide wire into the stomach and must mark the structure position outside of the chest by a thin metal piece.
- Slightly insert bougie on a guide wire to pass stricture, when bougie difficulty passes by resistance or bleeding appears,must stop pushing bougie because of a high risk of esophageal perforation [3, 4].
Esophageal stricture is dilaled by bougie through the mouth or gastrostomy hole. Bougies develop an axial force along the esophagus, so bougie dilation has a high risk of perforation compared to balloon dilation. Besides that, bougie can insert the mouth by blind method without a guide wire [2], however, this method shows an extreme risk of perforation, should not be applied.
To ensure safety, the “rule of three” is respected for bougie dilation, no more than three dilatator of sequential size with diameter over 1 mm per session if appearance of a moderate resistance [1].
1.2.2. Balloon dilation
Devices:
- Balloons can be used directly in the working channel and it is called the TTS system (“through the scope”). However, the maximum diameter of dilation is 8mm for 2.8mm channel and 12mm for 3.5mm channel. Balloon catheter has various sizes, a guide wire, C-am and contrast agent [2].
- Or larger balloon catheter, maximum 20mm of diameter is introduced on the guide wire by mouth into esophageal stenosis, then a 5mm small endoscope is inseretd beside the balloon to control the positioning of balloon, size of stricture during dilation process [2].
- Pump 1-2ml silicone into the working channel before insertion of balloon [5].
Steps of dilation procedure:
- Perform endoscopy to examine: position, size stricture, related lesions.
- Introduce a guide wire through the working channel.
- Insert balloon catheter on the guide wire.
- Mark the stenosis positioning by a metal piece.
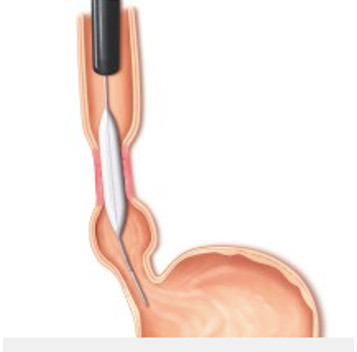
Control the positioning of the balloon at stenosis by using C-am (pumping contrast agent) [1, 3], the disappear of balloon waist. Hence, this waist can be observed on endoscopic screen by small endoscope or standard endoscope with the balloon catheter passes through the working channel [2].
- The balloon is inflated at stenosis, it combines with an observation of the expansion of the balloon.
The benefit of the observation under the endoscope screen is that the endoscopist can directly observe the efficacy during the dilation process [2]. Dilation can be a pneumatic balloon or water balloon.
Water balloon is only used to dilate a short stenosis: pumping water with a contrast agent to inflate the balloon and maintaining time is 1-3 minutes with the same pressure [3]. Nowadays, this technique is not common application due to the complexity, it requires C-am and health staff must work under a poisoned environment of X-ray.
Pneumatic balloon dilation: Nowaday, esophageal dilation by pneumatic balloon is a common indication and can be applied with benign esophageal stenosis (gastroesophageal reflux, caustic ingestion, and post-surgery of esophageal atresia which is recently recommendation). Dilation Time is in 30 seconds, if performing 3 continuous times in a session, total time does not exceed 1 minute [5]. The diameter of the pneumatic balloon is not 2mm bigger than the stenosis diameter. The inflation diameter of a balloon does not exceed 3 times compared to the stenosis diameter. In general, dilation is safe when implementing the 3 times dilation persession and the stenosis diameter after dilation increases properly around 3mm [1].
This technique has been applied popularly in our endoscopy department of Vietnam.
Dilationplanis common can be every 2-3 weeks, the symptoms of dysphagia will disappear if the stenosis diameter is 12mm [5].The advantage dilates uniformly the stenosis with local stationary radial force owing to balloon inflation without a lot of esophageal movement. The percentage of symptom reduction after esophageal dilation achieves 100-70% withcongenital or acquied malformation [2].
.jpg)
The exact number of dilations for esophageal stenosis is not recommended, it depends on the efficacy of the first dilation, type and size of stenosis [2]. However, the frequency of esophageal dilation for patients with gastroesophageal reflux disease base on the improvement of esophagitis and result of the first dilation [3].Patients often wake up in 6 hours after dilation, are always closely supervised to prevent complications and treated by omeprazole to avoid relapse [5]. Treatment by using antisecretory medication after dilation plays a role to decrease the risk of stenosis recurrence and is necessary for the next dilation. In cases with benign esophageal stenosis or treatment failure,new technical using is the injection of corticoid at stenosis area after dilation has showed a good result [1] or installing stents or dilation by using bougie with a guide wire.
.jpg)
Esophageal stenosis dilation is the most common technique in clinical practice. Esophageal and rectal stenosis dilation are performed more easily comparing to dilation at deeper position of gastrointestinal tract such as duodenum, colon and intestin. Phan Thi Hien, et all, 2008 had reported a girl child with 2 months of age, 2.8kg who was dilated at duodenal anatomosis by endosopy, the technique was safely and success [7].
1.3. Complications
The percentage of perforation related to benign esophageal strictures is approximately 3%. Complications happen easily when the size of balloon is not appropriate and prolong dilation time, especially in children with complex stenosis [5]. Furthermore, using balloons without guide wire also increases the risk of perforation. Hence, we always have to adhere strictly steps of esophageal dilation process and do not delete any steps.
If susspected of esophageal perforation, it is needed to perform esophagogram. The patient can eat again after dilation 24 hours if lacking the syndroms to refer complications [2]. If the patient presents symptoms of perforation, have to consult surgerons, however, medical treatment oftenly shows good results after 7-14 days, the patient is required fasting and intravenous nutrition, proton pump inhibitor and broad-spectrum antibiotic to prevent mediastinitis [5].
Under over 10 years of my experiences, I recognize that bougie without guidewire leads to a high risk of perforation because losing control of direction of bougie and pressure at stenosis position. Hence, i don’t recommend using this method at Vietnam National Children’s Hospital. Balloon dilation with guidewire has shown effective and safe results in patients with clinical symptoms due to esophageal stricture.
2. CARDIA DILATION
2.1. Indication
Cardia dilation is indicated in achalasiapatients; it is a special indication by using pneumatic balloon dilation. If this method has a successful result it will replace Heller surgical myotomy, especially in adults the success rate is 77%. Cardia dilation is usually used in children over 10 years old [3].
2.2. Technique
Patients need fluid feeding 48-72 hours before dilation and an esophagram with an image of achalasia. Candida treatment is necessary to prevent Candida transmission into mediastinum in perforation when mucosal biopsy showed Candida injection in achalasia patients [3].
Equipments: Rigiflex (Microvasive) dilatorincludes one balloon with two catheters, pushing balloon to slip on the guide wire, diameter of catheter is 5mm, length of balloon is 10cm and diameter of balloon is 30-40mm, using cylinder to pump 60ml air to inflate the balloon [3]. Using balloons with a diameter of 35-40mm and 500mm Hg pressure to allow the rupture of the muscular layer, usually each patient needs at least two or three sessions [2].
There are two techniques of cardia dilatation including a classic technique with C-am (fluoroscopic-guided) and a new technique without C-am (endoscope guided). This dilatation causes pain, so general anesthesia is required, but without muscule relaxants. This technique works by rupturing of somes fibers of the circular muscle incorporated in at lower esophageal sphincter.The amount of muscle ruptured depends on the pressure and diameter of the balloon as well as dilation time [5]. The steps of two techniques are similar, including:
- Perform endoscopy to examine cardia, release absolutely fluid and food, then push the endoscope into the stomach.
- Insert a guidewire through the working channel into an antrum under the control of endoscopy.
- Withdraw endoscope while the guidewire is still kept in the stomach.
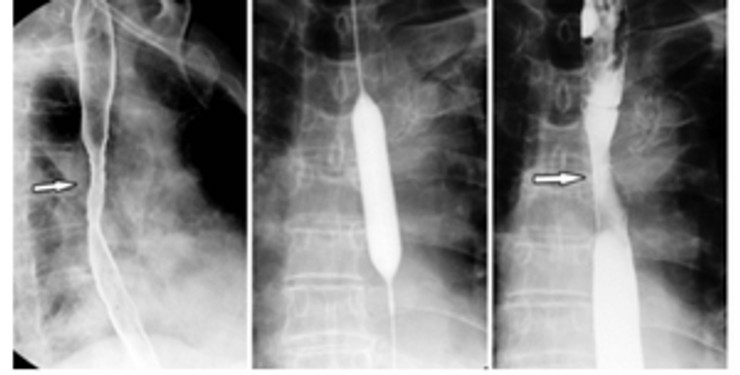
The next steps of dilatation in achalasia under C-am:
- Pushing the balloon slips on guidewire into cardia under control by using C-am (pumping a little contrast agent into the balloon).
- Based on the image of the contrast agent at the upper and lower part of the balloon, marked the position of cardia at corresponding point on the chest while performing endoscopy.
- Inflate the balloon gradually at the position of lower esophageal sphincter, endoscopists need to lightly pull the balloon to ensure it locates at the right position during the inflation process. At this time, an area with high pressure at lower esophageal sphincter is created, an image of the balloon is seen similar in appearance to a sandy watch at waist of the balloon, the pressure reaches 7-12psi.
- For optimal processes, the endoscopist only inflates the balloon with a diameter of 30mm during 45 seconds in children aged under 12 years old. In older children, initial time of inflation is 30 seconds and using the balloon with diameter of 30mm and then 15seconds with the balloon size of 35mm [5].
The next steps of cardia dilation (without C-am): DO NOT APPLY THIS TECHNIQUE IN CHILDREN:
- Marking a mid-section of balloon dilator with the thick colored macker.
- Passing the balloon over the guidewire into the stomach.
- Endoscopy to control the position of the balloon in the esophagus.
- Pulling the balloon back in the esophagus until the color mark reaches the gastroesophageal junction.
- Pump the balloon until it reaches a pressure of 12psi and maintain the pump until the appearance of an ischemic ring at the lower esophageal sphincter and stop pumping.
- Absolutely air suction from the balloon and withdrawing the balloon, dilation process is completed.
- Pump a small amount of contrast agent into the esophagus to control the leaking due to esophageal laceration.
Each patient is usually dilated 2-3 sessions. The result of dilation is like an achievement of a surgery method or better. In failure cases after 3 sessions, surgical myotomy is needed and the result of surgery is not affected by previous dilations [2].
According to recommendations of the American Society for Gastrointestinal Endoscopy, treatment by Botulinum toxin is an endoscopic method which can be use in cases if surgical response is not good in achalasia patients [1, 2].
2.3. Complications
In fact, we cannot exactly predict the time and pressure in special patients. Furthermore, using a high pressure, big diameter of the balloon and prolonged time of procedure lead a high risk of esophageal perforation immediately or later due to anemia leading to esophageal mucosal necrosis. Therefore, esophagogram immediately dilation to examine esophagus is needed, however, a false negative result can happen and monitoring is necessary. Prolong time of dilation increases a risk of perforation [5].
Esophagogram after dilation procedure is compulsory and the patient needs closely monitoring during 4 hours after dilation.Chest pain over 1 hour and fever are warning signs of a high risk of complication and the patient must to bepreventive treated immediately, should not wait for the sign of pneumomediastinum. A preventive treatment includes antibiotics, antisecretory drugs, absolutely fasting, intravenous nutrition, surgical consultation and early surgical indication if necessary [5].
The percentage of perforation is 2-4% of casesfor cardia dilatation and usually appears within 5 hours after dilation with post sternum and epigastric pain. This perforation is located under of cardia and left side of lower esophagus. Treatment is operation to manage laceration and perform Heller myotomy [3]. The mortality rate is approximately 0,5% [2].
The research results of Phan Thi Hien et al. (2018) showed that pneumatic balloon dilation is an effective and safe method to treat esophageal stricture after surgery of congenital esophageal atresia in children.
REFERENCES
1. James VE, Todd HB, Douglas GA et al (2006), “Esophageal dilation”, Gastrointestinal endoscopy, 63(6), 755-760.
2. Victor LF (2008), “Gastrointestinal Endoscopy”, Pediatric gastrointestinal desase, 2(1), 1259-348.
3. Mougenot JF (2000), “Endoscopie digestive”, Gastroentérologiepédiatrique, (2), 664-685.
4. Phan ThịHiền (2017), “Nong hẹp thựcquản, tâmvị”, Các qui trình kĩ thuật nhi khoa thường gặp, Nhà xuất bản Y học, 2, 383-385.
5. Gershman S (2012), “Therapeutic upper GI endoscopy”, Practical pediatric gastrointestinal endoscopy, 2(1): 82-103.
6. Kim JH, Shin JH, MD and Song HY (2010), “Benign Strictures of the Esophagus and Gastric Outlet: Interventional Management”, Korean J Radiol,11(5),497-506.
7. Phan Thị Hiền, Nguyễn Thanh Liêm (2008),”Nhânmộttrườnghợpđiềutrịhẹpmiệngnốitátràng ở trẻembằngnộisoi can thiệp”, Nghiêncứu y học, 57(4), 203-206.
8 Sanchis ML, Suárez-Callol P, Monzó-Gallego A et al (2015), “Management of primary achalasia: The role of endoscopy”, World J Gastrointest Endosc, 7(6), 593-605.
-

Self-design suction tool
20-05-2021 -

Removing phytobenzoar in Pig's stomach
20-05-2021 -

Remove twisting of the pig colon
04-05-2021 -

Pig stomach endoscopy
04-05-2021
-

Management of Ingested Foreign Bodies in Children: A Clinical Report of the NASPGHAN Endoscopy Committee
28-04-2021 -

Management of Familial Adenomatous Polyposis in Children and Adolescents: Position Paper From the ESPGHAN Polyposis Working Group
28-04-2021 -

Pediatric Colonoscopic Polypectomy Technique
28-04-2021 -

Gastrostomy Placement in Children: Percutaneous Endoscopic Gastrostomy or Laparoscopic Gastrostomy?
28-04-2021







