Phan Thi Hien, "Esophagus-stomach-duodenum endoscopy in children";, Medical Publishing House, Hanoi, Jan 2019 (page 151-163). Extract from specialty book: “NỘI SOI THỰC QUẢN – DẠ DÀY – TÁ TRÀNG TRẺ EM”, Nhà xuất bản y học, Hà Nội, ISBN: 978-604-66-3546-8.
INTRODUCTION
Esophagogastroduodenoscopy is indicated in cases with acute in upper gastrointestinal bleeding or recurrent bleeding without reason. Esophagogastroduodenoscopy is an optimal method to diagnose and can find the reasons for bleeding in 90% cases, especially it is indicated early in cases with bloody vomiting. Almost all children have upper gastrointestinal bleeding will be self stabilization, hence, emergency endoscopy is indicated when a patient has syndrome related to decision for medical or surgical treatment in emergency. Contraindications of endoscopy include patients in shock condition, hypovolemia, myocardial ischemia, or severe anemia [1].
Initial clinical diagnosis includes history and focus on quick assessment of general condition with vital signs. If having severe bleeding, immediate treatment before finding the reasons is necessary. Sensitive signs of gastrointestinal bleeding with circulatory collapse such as: tachycardia, then hypotension. Emergency solutions are bolus fluid and blood. If a patient
is not in a stable condition after infusion of ≥ 85ml/kg fluid or blood, needed indication for surgery. Surgical consultation is essential when a patient is having severe bleeding [1].
The average percentage of hemostatic endoscopic is 84-100% cases, the difficult cases are large chronic ulcers in the posterior wall of duodenal bulb or the superior angle of duodenum [2].
1. “Non-thermal” hemostasis
1.1. Epinephrine injection
* Indications:
- Gastrointestinal bleeding is not related to esophageal varices: beading by ulcer, arteriovenous malformation and after polypectomy.
- Injection of epinephrine can be a single application in management of bleeding such as bleeding by arteriovenous malformation, after polypectomy, or can combine with other methods such as thermal hemostasis or clipping device in ulcer or visibly bleeding vessel.
* Tools:
- Epinephrine In saline (1:10.000) is commonly used for patients with bleeding without esophageal varices, this method leads to vasoconstriction and compression into the bleeding vessel.
- Endoscopic needles 21-25 with short and 4mm length needles are commonly used, check the needle before using to prevent obstruction.
- Endoscopes have a biopsy channel of 2.8mm or 2mm of diameter.
* Technique [2, 3]
- Endoscopy to determine exact position of bleeding.
- Put a needle at right position, an assistant will push needle through out envelope to insert into mucosa (endoscopist always control perfectly needle under endoscopic screen).
- Assistant will pump and stop pumping epinephrine 1:10.000 according to the endoscopist's command, then withdrawing the needle into the envelope.
- Endoscopist continue to find other positions for injection.
- If the vessel is visible: injection in 4 angles around bleeding points, then one direct injection into the bleeding vessel.
- Or, directly injection into a bleeding vessel in the early stage of endoscopic management of bleeding. This technique is commonly applied in bleeding cases by arteriovenous malformation with hypovolemic shock or pedunculated polyp bleeding after cutting [2].
Notices:
- In adults: Total dose of epinephrine 1:10.000 ≤ 16ml per session and each injection ≤ 4 ml to avoid ischemia and perforation [2].
- In children: Total dose of epinephrine 1:10.000 normally is around 5-10ml per session divided into 4 injections [1]. To limit gastrointestinal ischemia and perforation, should inject around 4ml per session [4].
Epinephrine is a single therapeutic in management of bleeding and effective in 80-85% cases [1]. This method is priority in management of bleeding without esophageal varices [3] and we have applied it regularly in clinical practise, especially in bleeding caused by duodenal ulcer at difficult position to perform cliping technique.
1.2. Use clipping device to management of bleeding
In recent years, under advanced science development, metal clipping devices have been invented (clip). Application of using clip in acute gastrointestinal bleeding management in adults as well as children has shown good efficacy. This method provides physical strong compression to the bleeding vessel.
* Indications:
- Visibly bleeding vessel.
- Dieulafoy lesions [2].
* Tools:

- Clip: single-use rotatable clips for finding the optimal position which can be reopened and repositioned up to 5 times or only one time. Based on lesion, different opening clips can be used.
- Clipping tools have a metal spiral wire with 2.2mm of diameter covered by a plastic tube.
- Standard endoscopic has an interventional channel 2.8mm of diameter.
- In America, clips with 2 prongs are available (Resolution clip, Boston clip), they do not need covered plastic. This tool allows to suck and locate clip [2].
* Technique:
- Step 1 (install clip): Install clip into clipping tool (for reusable clip fixing devices) and then insert this tool through the accessory channel of the endoscope.
- Step 2 (activate clip):
+ Detect accurate bleeding point.
+ Determine accurate position to activate clip.
+ Opens the clip to its maximum diameter.
+ Shorten the distinction between clip and endoscopic tip.
+ Clipping bleeding point [4].
.jpg)
* Notices:
- One clip or more clips can be used per session.
- Do not force the clip to insert into mucosa before clipping.
- Always observe the clip in the middle of the lumen when the clip is opening because it (for reusable clip fixing devices) is easily split out while hitting the intestinal wall [4].
The most difficult practice by hemoclip is bleeding from a large chronic ulcer on the posterior wall of the duodenal bulb, or the superior duodenal angle. The efficacy of initial hemostasis for a bleeding ulcer or Dieulafoy lesion achieves 84-100%. Complications related to hemoclip are rare [2]. Do not recommend magnetic resonance imaging while a metal clip is installed.
Clipping technique is applied regularly in the Endoscopy department of Vietnam National Children’s Hospital, especially for bleeding after polypectomy. We recognize this technique is effective and easy to apply, however, this technique is limited and difficult to apply in duodenal bulb bleeding due to limited opening of clip and we must use epinephrine in injection in some cases.
Phan Thi Hien, et al. 2017 presented clipping technique was effective and has saved the lives of two infants who had gastrointestinal bleeding with high risk of death after surgical operation of congenital heart disease. Furthermore, the study showed that direct suction devices combined with standard gastroscope of adults in management of gastrointestinal bleeding in infants can reduce significant time to eliminate blood clots, it is an initial step to decide the success of interventional endoscopy. Both of these patients had a similar lesion in gastrointestinal tube, it was small erosion with 4mm of diameter in stomach or colon, and required bowel cleansing and carefully observed to detect the lesion [5]. Detailed evaluation suggested Dieulafoy malformation and showed under erosion.
2. Thermal hemostasis [2]
Indications: Bleeding without esophageal varices includes:
- Ulcer with bleeding vessel or non-bleeding vessel.
- Ulcer with an adherent clot.
- Mallory – Weiss tear with active bleeding.
- Vascular malformations or Dieulafoy’s lesions.
- Bleeding after polypectomy.
Three types of thermal hemostasis devices are used in pediatric practice.
2.1. Bipolar or multipolar thermal devices
- One clip or more clips can be used per session.
- Do not force the clip to insert into mucosa before clipping.
- Always observe the clip in the middle of the lumen when the clip is opening because it (for reusable clip fixing devices) is easily split out while hitting the intestinal wall [4].
The most difficult practice by hemoclip is bleeding from a large chronic ulcer on the posterior wall of the duodenal bulb, or the superior duodenal angle. The efficacy of initial hemostasis for a bleeding ulcer or Dieulafoy lesion achieves 84-100%. Complications related to hemoclip are rare [2]. Do not recommend magnetic resonance imaging while a metal clip is installed.
Clipping technique is applied regularly in the Endoscopy department of Vietnam National Children’s Hospital, especially for bleeding after polypectomy. We recognize this technique is effective and easy to apply, however, this technique is limited and difficult to apply in duodenal bulb bleeding due to limited opening of clip and we must use epinephrine in injection in some cases.
Phan Thi Hien, et al. 2017 presented clipping technique was effective and has saved the lives of two infants who had gastrointestinal bleeding with high risk of death after surgical operation of congenital heart disease. Furthermore, the study showed that direct suction devices combined with standard gastroscope of adults in management of gastrointestinal bleeding in infants can reduce significant time to eliminate blood clots, it is an initial step to decide the success of interventional endoscopy. Both of these patients had a similar lesion in gastrointestinal tube, it was small erosion with 4mm of diameter in stomach or colon, and required bowel cleansing and carefully observed to detect the lesion [5]. Detailed evaluation suggested Dieulafoy malformation and showed under erosion.
2.2. Computer-controlled thermal probe (heater probes) [2]
The device generates and controls heat and delivers pulses of energy through a silicon clip surrounded by a low heat-capacity metal envelope without any electric current in the tissue. The probe head is supplemented by three water jet systems.
The metal envelope warms up to the designed temperature in less than 0.2 seconds and cools off in less than 0.5 seconds. The computer has a role to control the temperature and total energy delivered to the tissue. The endoscopist makes a detailed program on the computer to deliver a specific amount of energy from 5 to 30J tailored to a specific bleeding lesion.
Advantages of the heater probe are:
- No direct contact between the probe and the tissue.
- Elimination of adherence to the tissue.
- Automatic control of energy delivered to the tissue.
- Can adjust depth of coagulation.
Bipolar/multipolar and heater probes are commonly used in America compared to other types of thermal hemostatic devices. These probes are available and they fit easily into the 2.8 biopsy channel. All these probes can provide adequate temperature for coagulation of mesenteric vessels up to 2mm in animal endoscopy [2]. Using a computer-controlled thermal probe in a bleeding ulcer is effective and safe, even in neonatal children [6].
2.3. Argon plasma coagulation [2]
- Plasma coagulation is the result of ionization of noble gas (argon), gas will fill in the space between electrical electrode and bleeding area.
- Ionized argon creates electrical current and maintains small and regular electrical current. The released energy leads to desiccation and coagulation without carbonization and evaporation, so it avoids deep tissue destruction.
- The depth of coagulation is related to the power setting of the machine and application time but almost no exceeding 3mm. Holding a probe in one site for 5 seconds with a power setting of 30-60W produces 2-3mm depth coagulation [2].
Advantages of hemostasis by argon plasma include:
- Larger area of coagulation than bipolar/multipolar probes [2].
- Decreased depth of tissue destruction [2].
- Control the deep level of coagulation [6].
The procedure can lead to perforation because the probe contacts directly with tissue, stretching the bowel wall due to the accumulation of argon in the stomach, or the intestine.
Thin (1.5mm) probes are commonly used in America and suitable for small caliber pediatric endoscopes, even this technique can deploy for neonates [2]. Two common types of complications in adults are perforation or submucosa emphysema because the probe directly contacts mucosa that makes argon flow go into and destroys tissue.
2.4. Technique of thermal coagulation [2]
- Step 1: Endoscopists have to understand devices and coagulation mode, then optimize treatment requirements for specific bleeding lesions to choose tools. High power and coagulation application settings should only be used for patients with severe dysplasia, should not deploy these modes in patients with ulcer because it has a high risk of perforation.
Hemostasis by using argon plasma is implemented based on specific cases.
- Step 2: Classification of bleeding from a nonvariceal lesion in the stomach or duodenum (artery or venous is observed or from tissue). During endoscopy, endoscopists see vessels appear as a pyramid like “island” at the base of the ulcer.
- Step 3: Optimal observation of bleeding point before intervention
+ If an observation of forceful pulsating eruption of blood from ulcer, this is arterial bleeding. Immediately, have to force pressure by bipolar or heater probe up against the bleeding vessel. Then, using 4 pulses of 30J of the heater probe or 8-10 seconds pulses with a power setting of 15-20W on a 50 W generator for bipolar or multipolar probe before repositioning the probe [2].
+ Coagulation process is deployed repeatedly until the vessel becomes flat and bleeding stops.
An adherent clot:
+ Challenge of removing a large blood clot at the bleeding point is a challenge because it has a high risk of worsening bleeding. Therefore, endoscopists need to carefully evaluate the potential benefits before removing this clot to expose a bleeding vessel.
+ Need cleansing out of blood and fibrin around ulcer to optimize observation.
+ Inject epinephrine around the adherent clot to prevent bleeding while removing a blood clot out of the ulcer.
+ This technique requires a high skill endoscopist and smooth coordination of the endoscopic team.
- Step 4: Hemostatic endoscopy by above methods
Complications commonly happen in cases without clear visible vessels, especially in active duodenal bleeding. Forceful irrigation and suction will limit complications. If the vessel stops bleeding temporarily, lesion is observed more clearly, the endoscopist determines the exact position of bleeding and chooses proper interventional tools. Thermal hemostatic devices have minimal value in ulcer without bleeding as well as well-organized flat clot, red or black spots or gray fibrin in the ulcer base [2].
The factors that lead to fail in hemostatic endoscopy for ulcer include: the diameter of ulcer > 2cm, hypovolemic shock, flat lesion and active severe bleeding. Endoscopy for cases with active severe bleeding should be deployed after 24 hours. In these cases, endoscopy can be a failure (5-8% in adults, no pediatric case was reported), surgery is needed to perform [1].
The combination between epinephrine injection and bipolar probe is a common application in hemostatic endoscopy for upper gastrointestinal haemorrhage in children [1]. At Vietnam National Children’s Hospital, clipping devices or epinephrine injection are commonly used for bleeding without esophageal varices.
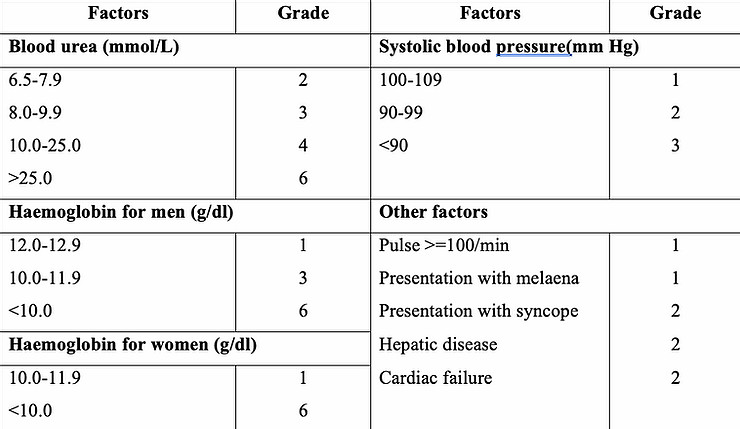
Some classifications are applied to prognosis upper gastrointestinal haemorrhage, such asGlasgow-Blatchford score is applied in adults [7]. Total scores of GBS≤ 2 points, the patient does not need emergency endoscopy and they are suitable for management at home. If the GBS ≥ 3, the patient has a high risk of interventional endoscopy or death.However, application of GBS in children has not been reported in study. Therefore, GBS contributes partly in
prognosis of gastrointestinal haemorrhage in children.
Generally, specific hemostatic methods are used in specific lesions, age, and it depends
on available devices. Hence, the most challenge of hemostatic endoscopy is a limited observation due to exceeding bloody fluid or adherent clots. Direct Suction devices (branch of US endoscopy) or our self made devices are extremely useful in these cases.
REFERENCES
1. Gilger M.A., Lynette K (2008), “Upper Gastrointestinal Bleeding”, Pediatric
gastrointestinal desase, (2), 1285-90.
2. Gershman G (2012). “Therapeutic upper GI endoscopy”, Practical pediatric
gastrointestinal endoscopy, (2), 82-103.
3. PhanThịHiền (2017), “Nội soi dạ dày thực quản dạ dày và tiêm cầm máu”, Các qui trình kĩ thuật nhi khoa thường gặp, Nhà xuất bản Y học, tập 2, 374-376.
4. PhanThịHiền (2017), “Nội soi cầm máu bằng clip trong chảy máu tiêu hóa”, Các qui trình kĩ thuật nhi khoa thường gặp, Nhà xuất bản Y học, tập 2; 394-395.
5. PhanThị Hiền, Trương Thị Mai Hồng (2017), Báo cáo hai trường hợp nội soi can thiệp chảy máu tiêu hóa sau phẫu thuật tim hở ở trẻ nhỏ, Tạp chí y học thực hành, 1050(7), 12-14.
6. Victor L.F (2008), “Gastrointestinal Endoscopy”, Pediatric gastrointestinal desase, 2(1), 1259-1348.
7. Recio-Ramírez JM, Sánchez-Sánchez MP, Peña-Ojeda JA et al (2015), “The predictive capacity of the Glasgow-Blatchford score for the risk tratification of upper gastrointestinal bleeding in an emergency department”, Revista Española de EnfermedadesDigestivas, 107 (5), 262-267.
-

Self-design suction tool
20-05-2021 -

Removing phytobenzoar in Pig's stomach
20-05-2021 -

Remove twisting of the pig colon
04-05-2021 -

Pig stomach endoscopy
04-05-2021
-

Management of Ingested Foreign Bodies in Children: A Clinical Report of the NASPGHAN Endoscopy Committee
28-04-2021 -

Management of Familial Adenomatous Polyposis in Children and Adolescents: Position Paper From the ESPGHAN Polyposis Working Group
28-04-2021 -

Pediatric Colonoscopic Polypectomy Technique
28-04-2021 -

Gastrostomy Placement in Children: Percutaneous Endoscopic Gastrostomy or Laparoscopic Gastrostomy?
28-04-2021







